Amazing natural alternative to antibiotics.
There is no disease-causing bacteria that can live in the presence of
even the slightest traces of metallic silver. The Best Colloidal Silver >> << contains only natural ingredients that help the body fight infections
as synthetic antibiotics, but without the damaging effects >> << parties. Its natural deep golden color characteristic of high quality >>. Concentration << twenty parts per million of silver contained
is very effective, safe design. Higher concentrations may
actually be less effective because they can interfere with beneficial strattera 40mg bacteria
discoloration of the skin and cause, even if for internal use. Each family >> << wanting the best natural health should have a bottle of Colloidal Silver >> << in the medicine cabinet. "Let me tell you that
when our kids were chicken pox, a few years ago, we spray her with
colloidal silver from head to toe, and most surprising was that the children
. no more itchy chicken pox ran its turn, but when
everything was over, there were no traces of ash yet we were very happy
those results. ". - SM "My daughter was >> << sore throat and fever 102ye. I spray her throat colloidal silver. Within 48 hours of sore throat and fever had disappeared. It was the first time
it never to return so quickly and without taking antibiotics
".
KB Silver in colloidal form
been proved useful against various infections and
non-toxic in reasonable concentrations of all species of fungi,
bacteria, protozoa, parasites and some viruses. Higher grade colloidal
SILVER conducted a technical electrocolloidal method using
electricity. It has a pH of about 6. 5 and is a natural
- deep golden color. During production, it contains 20 parts per million
hyperfine particles 99. 999% pure silver, 0. 0001 microns in diameter
electro-magnetic charge and suspended in deionized water. This is not the
to keep in the refrigerator. Silver particles in colloidal silver topovoyi >> << remain in limbo without any chemical substances, proteins,
stabilizer, or artificial additives. Typically, the antibiotic kills a half dozen >> << bacteria, but silver kills some 650. Resistant strains develop NOT
silver, as they do with antibiotics. Silver is used as a proven germ fighter
in the early 1900's. This was the basis of antibiotic treatment,
, and modern technology even better. Medical journal Lancet reported phenomenal results
colloidal silver in 1914. Dr. Henry
Crookes showed highly bactericidal colloidal silver is not quite
harmless and non-toxic to humans. Colloidal silver has been proven useful >> << against all fungi, bacteria, protozoa, parasites and some viruses
, often die within minutes. LC Ford, MD on
UCLA School of Medicine reported that in 1988 silver solutions were effective against
streptococcus, Pyogenes, Staphylococcus Aures, Neisseria
Gonorrhea, Garnerella, vaginal, Salmonella typhoid and other intestinal pathogens.
It also found that the fungicidal for Candida Albicans,
Candida Globata and M. Furfur. Science Digest said
in an article published in 1978 titled "Our Mightiest embryos Fighter", the "silver
becomes a miracle of modern medicine." Typically, the antibiotic kills
half a dozen bacteria, but silver kills some 650. Resistance
strains do not develop silver, as they do with antibiotics. Dr. Robert O. Becker
, the doctor said that "we have again the fact that silver kills bacteria
that have been known for centuries ... when antibiotics
found uses for silver as an antibiotic were discarded
".
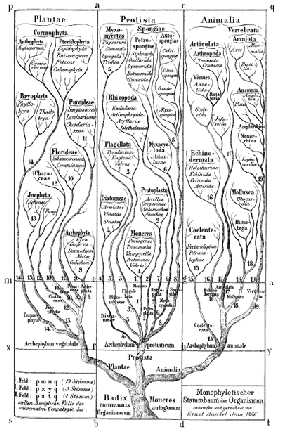
, Term "colloid" refers to substances
which consists of tiny particles. In the true colloids, these particles
can not be seen with the naked eye, and electric charge. The particles slightly larger than molecules and is measured in microns.
This activates antibacterial quality silver >>. << "Hammer" method can be used, but
particles are too large, and the protein or other stabilizers must be included
. However, regulators may impede performance. In addition,
chemical process can be used, but the end product is usually too acid and
not so effective. Best Colloid >> << SILVER conducted electrocolloidal process that allows a
small particles of silver to be suspended in a solution of tiny charge
placed on them. This process replaces the need for any chemicals or stabilizers
product and can be called a true colloid. Then the particle
can remain in suspension almost indefinitely. Advanced Colloidal Silver
perfect deep golden-yellow color. Other products that are not true colloids
is a different color if color is added. Color
critical indicator of quality colloidal silver. Silver may be due to the proper functioning of our immune system >> << and that people with inadequate intake may be more prone to infections >>. Higher grade << colloidal silver contains
99. 999% pure colloidal silver particles
, 0. 0001 microns in diameter with a concentration of 20 parts per million
having little impact on the friendly bacteria in the digestive tract >>. << However, be aware of products with higher concentrations, they can attack
friendly bacteria, and some antibiotics. This may disappoint
, your natural balance and lead to other complications. With colloidal silver
high concentration is not necessarily better. Indeed >> << opposite is usually true. Not all colloidal silver
has the same quality. Some that I actually bought was sour >> << smell and taste awful. It is important to be careful to buy
from a trusted source when buying any food. The best rule
: do not trust the labels! - Know the manufacturer! . << >>